Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder that affects individuals across the lifespan. Characterized by difficulties with attention, hyperactivity, and impulsivity, ADHD can have a significant impact on academic, occupational, and social functioning. Despite its prevalence and impact, ADHD remains widely misunderstood and stigmatized. This article provides a comprehensive overview of ADHD, including its causes and risk factors, impact on development and functioning, treatment options, how occupational therapy can help with ADHD, challenges and stigma, personal stories and perspectives, and future directions and research. By exploring the complexities of ADHD and highlighting the experiences of individuals with the disorder, this article aims to promote greater awareness, understanding, and support for those affected by ADHD.
The CDC uses datasets from parent surveys and healthcare claims to understand diagnosis and treatment patterns for attention-deficit/hyperactivity disorder (ADHD). Estimates for diagnosis and treatment can vary depending on the source. This page includes ADHD data from different sources.
The estimated number of children aged 3–17 years ever diagnosed with ADHD, according to a national survey of parents,1 is 6 million (9.8%) using data from 2016-2019. This number includes:
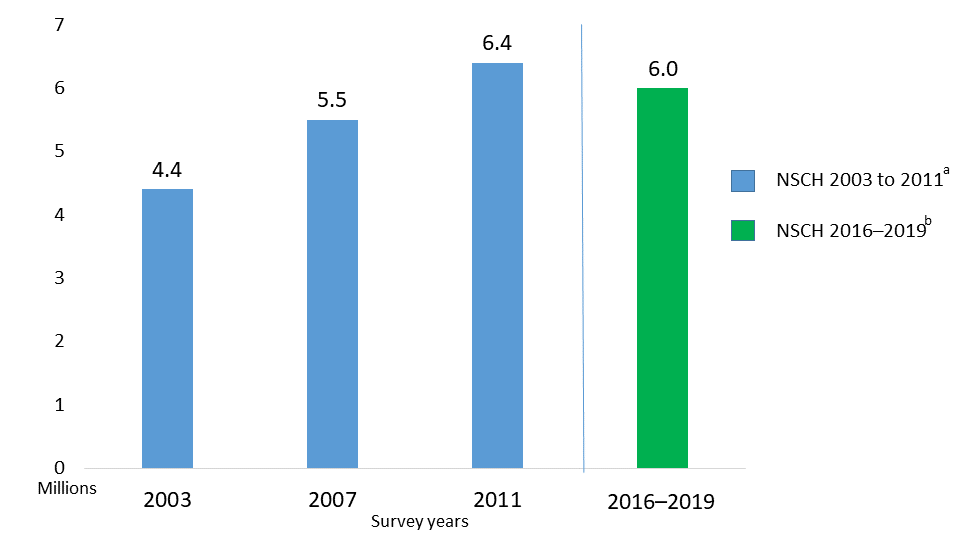
ADHD diagnoses rates have changed over time. The charge below shows the total number of people diagnosed with ADHD from 2003 to 2019. New Jersey is at the lower end of the prevalence range with a 7.9% diagnosis rate, whereas Louisiana has the highest diagnosis rate at 16.3%.
According to the Mayo Clinic, The primary features of Attention Deficit Hyperactivity Disorder include inattention and hyperactive-impulsive behavior. ADHD symptoms start before age 12, and in some children, they're noticeable as early as 3 years of age. ADHD symptoms can be mild, moderate or severe, and they may continue into adulthood.
ADHD occurs more often in males than in females, and behaviors can be different in boys and girls. For example, boys may be more hyperactive and girls may tend to be quietly inattentive.
There are three subcomponents to ADHD. Three major types of ADHD include the following:
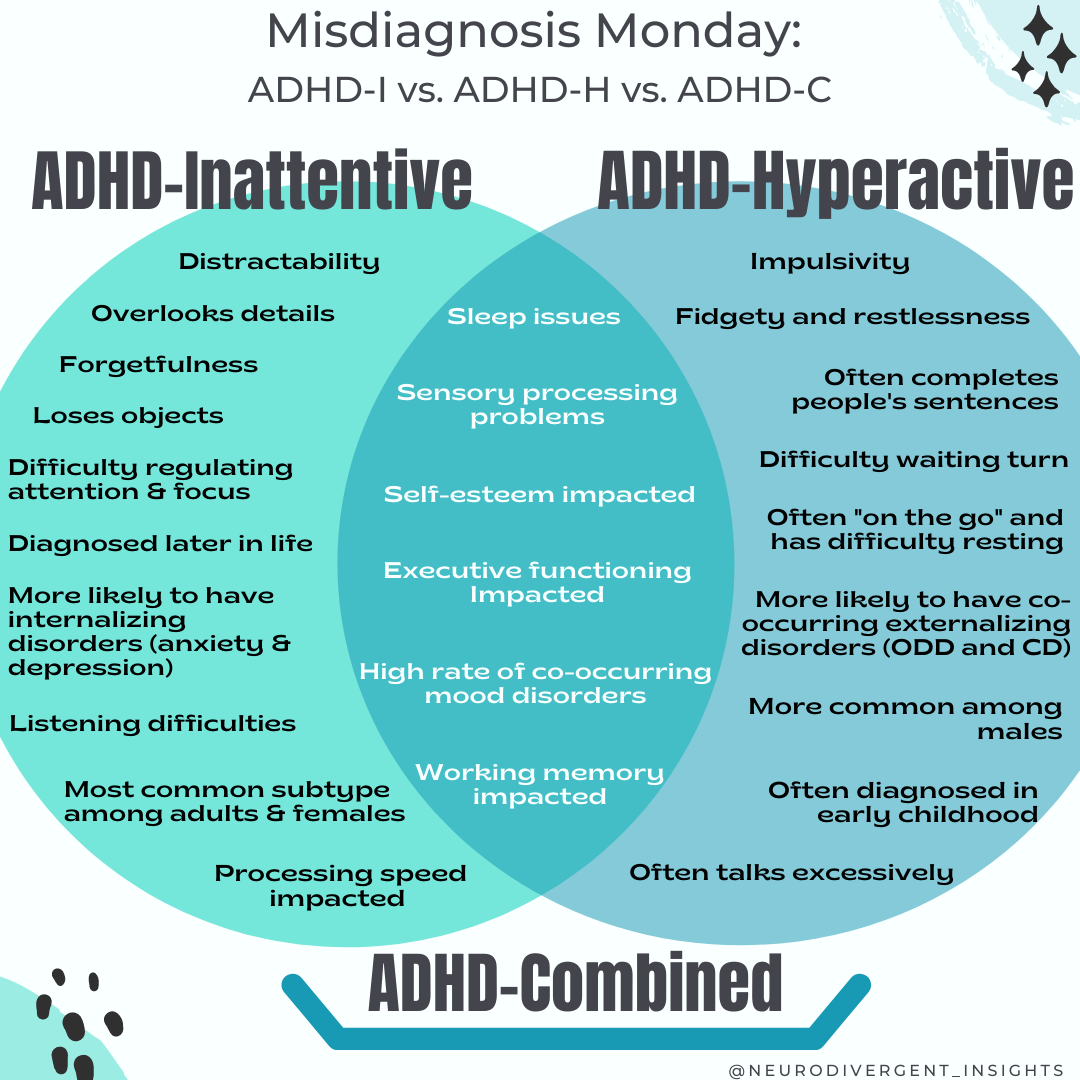
Working memory and processing speed are often impacted in the context of ADHD-inattentive type (processing speed may not become impacted until too many tasks are placed on the person). This type is the most common type diagnosed among adults and females.
ADHD-inattentive type (formally known as ADD) is marked by:
Inattentive Attention Deficit Hyperactivity Disorder does not look like the stereotypical presentation of ADHD. Most people think of a young child who is struggling to sit in their seat or running around tirelessly. However, ADHD-I can look like:
ADHD-Hyperactivity is the most common form of ADHD diagnosed in preschoolers. It is associated with behavioral difficulties in early childhood and co-occurs with Oppositional Defiance Disorder (ODD) and Conduct Disorder (CD) at high rates (Bendiksen et al., 2014). ADHD-H is characterized by the need for constant movement. Such folks often fidget, squirm, and get up from their seat to walk around or stand. Children with ADHD-H are often described as if they are “driven by a motor” (running around excessively).
Hyperactivity may also show up as excessive talking, difficulty waiting their turn, and difficulty with self-control may lead to impulsive behaviors (blurting out answers, engaging in risky activities, and so forth). This type of ADHD is the most recognizable and thus diagnosed more readily than ADHD-I. It is more commonly diagnosed among children and men.
ADHD-C has a high prevalence rate and is the most common presentation among children.
Combined type ADHD is diagnosed when a person presents with six out of the nine symptoms of both inattention and hyperactivity. ADHD-C also co-occurs with externalizing disorders such as ODD and CD at high rates (Bendiksen et al., 2014). People with ADHD-C often have co-occurring internalizing disorders (anxiety and depression).
ADHD is diagnosed through a comprehensive evaluation that typically involves gathering information from multiple sources, including the individual, their family members, teachers, and other healthcare providers. The evaluation may include the following steps:
It is important to note that the diagnostic process for ADHD can be complex and may require multiple appointments with a healthcare provider who specializes in ADHD. It is also important for the individual and their family members to provide as much information as possible to assist with the diagnostic process.
Although the precise causes of ADHD are not yet fully understood, research suggests that a combination of genetic, environmental, and neurological factors may contribute to the development of the disorder.
In addition to these factors, research has also identified several risk factors that may increase the likelihood of developing ADHD, including:
Although genetics and brain structure are thought to play a significant role in the development of ADHD, environmental factors such as prenatal and perinatal complications, exposure to toxins, and psychosocial stressors may also contribute to the disorder. Identifying these risk factors and understanding their interplay is critical for developing effective prevention and treatment strategies for individuals with ADHD.
Early detection and diagnosis of Autism Spectrum Disorder (ASD) is crucial for several reasons:
Overall, early detection and diagnosis of ASD can have a significant impact on the developmental outcomes and long-term quality of life for individuals with ASD and their families. It is important for healthcare providers, educators, and families to be aware of the signs of ASD and to seek evaluation and diagnosis as early as possible.
Attention-deficit/hyperactivity disorder (ADHD) can have significant impacts on a child's development and functioning. The symptoms of ADHD can manifest in several different ways and can affect multiple domains of a child's life, including academic, social, and emotional functioning.
It is important to note that the impacts of ADHD on development and functioning can vary from child to child and depend on factors such as severity, subtype, and comorbidities. Early identification and intervention are critical for supporting children with ADHD and mitigating the potential negative impacts of the disorder. A comprehensive treatment plan may include behavioral interventions, medication, educational accommodations, and support for parents and caregivers. With appropriate treatment and support, children with ADHD can thrive and reach their full potential.
The bulk of treatment research on ADHD has focused on the condition in children, and the options for them have a strong evidence-base for symptom reduction. For many, the need for intervention persists over the long-term. Research from the landmark National Institute of Mental Health Multimodal Treatment Study of ADHD showed significant improvement in behavior at home and school in children with ADHD who received carefully monitored medication in combination with behavioral treatment. These children also showed better relationships with their classmates and family than did not children receiving this combination of treatment. Further research confirms that combining behavioral and stimulant treatments are more effective than either treatment alone.
Treatment plans are typically tailored to each child’s specific needs and may involve a combination of interventions.
It is important to note that treatment for ADHD is not one-size-fits-all, and what works best for one individual may not work for another. It may take some time and trial and error to find the most effective treatment plan. It is also important to regularly monitor and adjust treatment plans as needed to ensure continued effectiveness. With appropriate treatment and support, individuals with ADHD can lead successful and fulfilling lives.
Attention-deficit/hyperactivity disorder (ADHD) can present several challenges for individuals living with the condition. In addition to the core symptoms of inattention, hyperactivity, and impulsivity, individuals with ADHD may also struggle with other issues, including social difficulties, anxiety, depression, and low self-esteem. These challenges can impact a person's academic, occupational, and social functioning and may contribute to stigma and misunderstanding surrounding the condition.
One of the main challenges associated with ADHD is the negative stigma that can be attached to the condition. Many people with ADHD may be seen as lazy, unmotivated, or lacking willpower, when in reality, their struggles are due to underlying neurological differences in their brain function. This stigma can lead to social isolation, discrimination, and reduced access to necessary resources and support.
Another challenge for individuals with ADHD is the potential for academic and occupational difficulties. Children with ADHD may struggle with organization, time management, and completing tasks, which can lead to poor academic performance and frustration for both the child and their parents. Similarly, adults with ADHD may have difficulty with workplace tasks and may struggle to meet deadlines or stay focused on important projects.
Furthermore, ADHD can also impact social functioning, as individuals with ADHD may struggle with impulsivity, emotional regulation, and social communication. This can lead to difficulty forming and maintaining relationships, as well as social isolation and loneliness.
In addition to these challenges, there are also many misunderstandings about ADHD. Some people may view ADHD as a made-up condition or believe that it is overdiagnosed. This can make it difficult for individuals with ADHD to receive appropriate diagnosis and treatment, as well as lead to feelings of shame or self-doubt.
It is important to understand that ADHD is a real condition that can have significant impacts on a person's life. While there may be challenges and stigmas associated with the condition, there are also many resources and supports available to help individuals with ADHD thrive. With appropriate treatment and understanding, individuals with ADHD can lead successful and fulfilling lives.
The below video helps explain what is like for a child with ADHD.
Occupational therapy (OT) can be a valuable treatment option for children with attention-deficit/hyperactivity disorder (ADHD). OT is a holistic, patient-centered approach that focuses on improving a person's ability to perform everyday tasks and participate in meaningful activities. For children with ADHD, occupational therapy can address a range of challenges related to the condition, including difficulties with attention, organization, and self-regulation.
Here are some ways in which occupational therapy can help children with ADHD:
Overall, occupational therapy can be a valuable tool for children with ADHD, helping them to develop skills and strategies that can improve their daily functioning and quality of life. By focusing on the child's individual needs and strengths, occupational therapists can create tailored treatment plans that address the unique challenges of ADHD.
In conclusion, understanding attention-deficit/hyperactivity disorder (ADHD) is crucial for recognizing and addressing the challenges faced by individuals living with the condition. ADHD is a neurodevelopmental disorder that impacts attention, organization, and self-regulation, and can have a significant impact on daily functioning and quality of life.
The causes and risk factors for ADHD are multifactorial and complex, involving genetic, environmental, and neurobiological factors. While there are effective treatments available, including medication, therapy, and lifestyle interventions, there are also stigmas and misunderstandings surrounding the condition that can impact access to appropriate care and support.
Occupational therapy is a promising treatment option for children with ADHD, offering a holistic and personalized approach that addresses a range of challenges related to the condition. Sensory integration therapy, organization and time management strategies, social skills development, play therapy, and physical activity can all be effective interventions for improving the daily functioning of children with ADHD.
Looking ahead, there is still much to be learned about ADHD, including how to improve early identification and intervention, and how to better understand the underlying neurobiological mechanisms involved in the disorder. Additionally, continued research into the effectiveness of existing treatments and the development of new interventions is necessary to improve outcomes for individuals with ADHD.
By increasing our understanding of ADHD, we can reduce stigma, improve access to care, and help individuals with the condition reach their full potential. With continued research, education, and support, we can work towards a more inclusive and understanding society that recognizes the diverse needs of individuals with ADHD.
1801 E 2nd St.
Scotch Plains, NJ 07076
Serving Westfield, Cranford, Berkeley Heights, Watchung, New Providence, and Summit